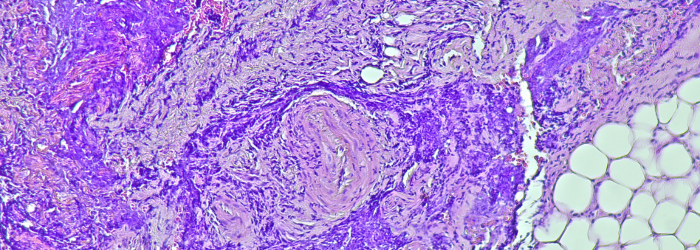
A 2024 study by Halpin-Veszeleiova et al. addresses one of the most persistent barriers in solid tumour immunotherapy: hypoxia-induced immunosuppression. The authors present a novel and clinically feasible strategy to reverse tumour hypoxia using a perfluorocarbon (PFC)-based oxygen-carrying nanoemulsion, combined with respiratory hyperoxia.
By directly targeting the hypoxia-adenosinergic immunosuppressive axis, the therapy improved the infiltration and cytotoxic function of T cells and NK cells, leading to tumour regression and improved survival in murine cancer models. Their work offers strong preclinical justification for using oxygenation agents as adjuvants to immunotherapy, particularly adoptive cell transfer (ACT).
How the Whitley Hypoxystation Enabled This Research
A critical element of this study was the ability to accurately replicate tumour hypoxia in vitro. This was achieved using the Whitley H35 HEPA Hypoxystation, which provided:
Precise, Stable Low Oxygen Conditions
- The Hypoxystation was maintained at 1% O₂, 5% CO₂, and 37°C, simulating the severe hypoxia found in the tumour microenvironment (TME).
- This level of control was essential for pre-conditioning samples and validating oxygen-carrying capacity in a physiologically relevant setting.
In Vitro Evaluation of Oxygenation Agents
- The authors exposed their PFC nanoemulsion (Perflubron) to 100% oxygen, then assessed its ability to release oxygen in a hypoxic environment using PreSens oxygen probes.
- These experiments were conducted inside the Hypoxystation, allowing the team to compare saturated vs. unsaturated formulations under controlled 1% O₂ conditions.
- The results confirmed that oxygen-preloaded Perflubron significantly elevated and prolonged oxygen availability under hypoxia-crucial data for therapeutic planning.
Enhanced Data Reliability
- The closed, HEPA-filtered environment of the H35 workstation ensured consistent atmospheric conditions during extended experimental runs -eliminating variability caused by transient oxygen exposure.
Figure 1C in the paper directly credits the Whitley H35 Hypoxystation for enabling these measurements, which underpinned the experimental strategy.
Scientific Significance
The research demonstrated that:
- Hypoxia suppresses antitumor immunity by upregulating adenosine, HIF1α, and A2A receptor-mediated pathways.
- Eliminating hypoxia, via oxygenation agents and respiratory hyperoxia, reversed this suppression and enhanced immune cell infiltration and activity.
- ACT efficacy was significantly improved, suggesting translational value for patients with hypoxia-rich tumours.
These discoveries are particularly relevant for tumour types resistant to checkpoint inhibitors, where hypoxia-induced barriers often persist despite immunotherapy.
Why This Matters for Hypoxia Research
This paper exemplifies how oxygen control is no longer a luxury, but a necessity in immunological and oncology research. Accurate oxygen regulation is vital for:
- Modelling pathophysiological conditions (like tumour hypoxia).
- Validating therapies aimed at reoxygenation.
- Understanding how immune cells behave in oxygen-limited environments.
The Whitley Hypoxystation enabled these researchers to go beyond speculative models and deliver data that closely mimics in vivo tumour conditions.
This paper highlights an important development in cancer immunotherapy research, made possible by the use of the Whitley Hypoxystation. The ability to tightly regulate oxygen conditions in vitro allowed the authors to demonstrate how reversing hypoxia can reinvigorate immune responses and enhance the effects of adoptive cell therapy.
As hypoxia remains a key hurdle in cancer treatment, the Whitley Hypoxystation continues to be an essential tool in the fight to understand and overcome oxygen-driven immune suppression. For more information on our range of Hypoxystations, please browse the products below or, to read to full paper head over to our published paper database.


 en
en
 xEnglish
xEnglish